Essentials of a Disc Herniation & Bulging Discs
Back pain affects nearly everyone at some point in their life. For some of us that are unlucky, this pain can be very severe and affect nearly everything we do in our lives. One of the most sudden causes for severe back pain is suffering a slipped disc, medically known as a disc herniation. Below we cover some of the important things to know about this condition and
What is slipped disc?
The spinal column in the human body is made of a series of irregular bones called vertebrae, which essentially provide protection to the spinal cord. Descending from the neck, your vertebral (spinal) column comprises of seven cervical vertebrae, twelve thoracic (mid-back) vertebrae, five lumbar (lower back) vertebrae, the sacrum and the base, which is known as the coccyx.
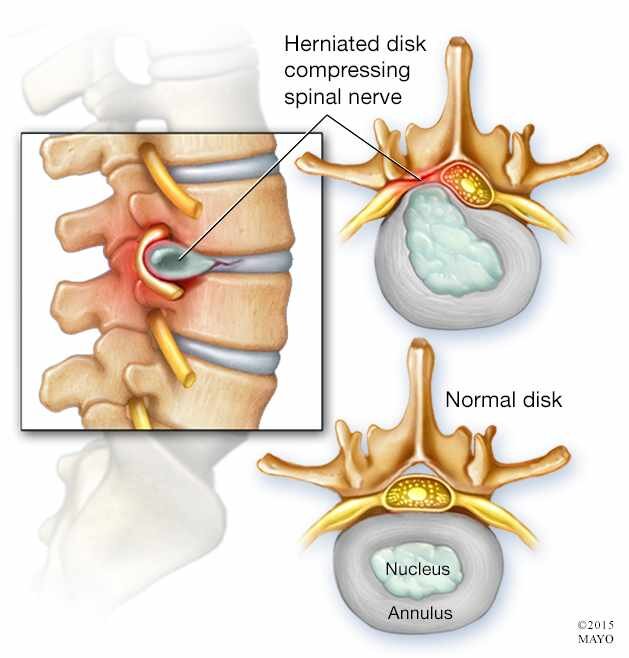
These vertebral bones are padded by intervertebral discs, which act as shock absorbers during activities like walking, bending, lifting, and twisting. The disc is made up of a soft and gelatin like inner part and a tough outer part. Injury to the spinal cord or spinal weakness can result in protrusion of the inner part of the disc through the outer part. This is termed as slipped disc, spinal disc herniation or disc prolapse.
What does slip disc pain feel like?
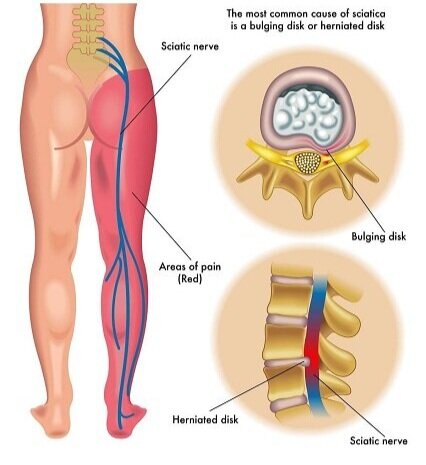
Spinal disc herniation or slipped disc pain usually starts as lower back pain, wherein it may also be termed as lumbar disc herniation and may radiate to both the lower limbs. You may have stiffness in your low back causing restriction of movements. The pain is usually sharp and excruciating. Mostly you will feel pain in the hips, thighs and calf muscles. Cervical disc herniation on the other hand, may manifest as localized pain in the neck and shoulders and also maybe associated with weakness or numbness in your arms and fingers. Intervertebral disc herniation symptoms may also include pain associated with numbness and tingling. People with disc herniations find it difficult to walk for a prolonged period of time and usually experience pain even when walking short distances. Slipped disc pain also worsens at night or with certain movements with a burning, tingling and achiness felt in the affected area.
What causes slip disc pain?
Protrusion of the inner soft part of the disc through the outer part is termed as slipped disc. Herniation of lumbar spine (L5) and sacrum (S1) usually causes nerve compression and is termed as L5-S1 disc herniation. Paracentral disc herniation is the most common (90-95%) type of herniation affecting the lower nerve root at L4-L5. When a large part of your disc displaces beyond its normal limit it is termed as bulging disc. But in disc herniation, less than 25% of disc dislodgment occurs. As you age, your discs start to desiccate and shrink in size. Due to the normal break down process of your disc, degeneration starts within the disc and the protective water content may gradually come down, causing the discs to slip more easily out of place. The second most common cause of slip disc after old age is mechanical injuries and accidents. Other causes of slip disc pain would include lifting a very large or weighty item, being overweight, frequent driving, sedentary life style, smoking (as it decreases the oxygen supply to the disc and hastens degeneration), etc.
What is the diagnostic tool for slip disc?
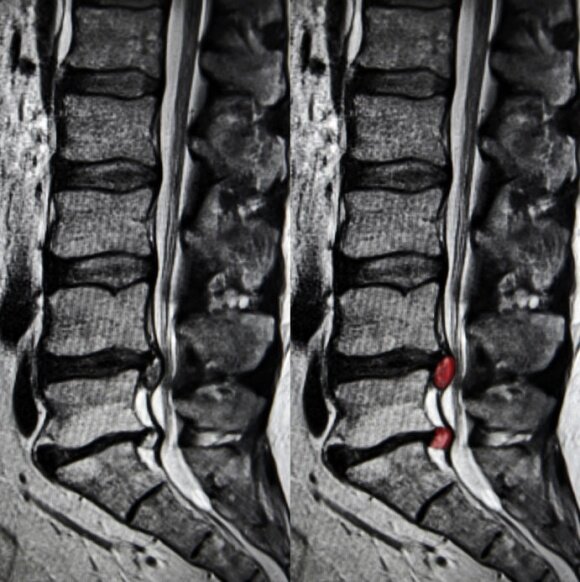
Your healthcare provider would first perform a detailed physical examination to assess the source of your discomfort. This would include a neurological exam and also an assessment of the nerve function and muscle vitality and strength. Range of motion tests would also be performed to assess the degree, severity and origin of the slip disc. Radiological studies would include x-rays, MRI, CT-scan, and discograms.
What are the treatments for slip disc?
It is usually seen that 90% of patients show signs of improvement within three months with non-operative care with a decrease in the size of herniation over time (reabsorption takes place). The most recent advancement of non-surgical care for slipped discs include spinal decompression therapy. Spinal decompression has come a long way in recent years, showing greater results for slipped discs as the decompression equipment evolves. Other conservative care includes physical therapy, extension exercises, chiropractic manipulation, bed rest followed by progressive activity as tolerated, non-anti-inflammatory medication, muscle relaxants, narcotics and oral steroids. Your body’s immune responses (macrophages) also play an important role in removing the dying or dead cells. In case the non-surgical management fails, selective nerve root corticosteroidal injections are another option. Surgical intervention would include laminotomy and discectomy.
When should I see my Doctor?
You should see the doctor when your back pain has been bothering you and not responding to over-the-counter painkillers or when you find yourself incapable of performing certain activities or movements that you had been able to in the past. If the low back pain and symptoms start getting worse and/or not improving or if the pain is associated with the below mentioned “red flags”:
The risk is higher when your age is under 20 or above 55.
If light tapping causes pain over low back area.
Associated with fever and chills of unknown cause.
Associated with numbness and tingling in legs.
Associated with weight loss.
Associated with difficulty in urination, involuntary urination, numbness around the groin, foot drop, and weakness in lower limbs (all these are probable signs of a neurological connection).
What are the risk factors for slip disc?
About 90% of your bone mass is acquired by the age of 20 years and your bones begin to lose their bone mass around the age of 40. The following are the risk factors for slip disc if
You are under 20 or above 50 years
If your job entails more of lifting and carrying heavy items or forward bending activities.
Individuals who are overweight and taller
Smoking is an important cause of spinal disc herniation as the nicotine and carbon monoxide prevent the disc cells from absorbing nutrients from the blood. This could lead to desiccation and dehydration of the discs, leading to degeneration.
Lack of physical exercise, a sedentary lifestyle may cause your muscles to become weak and put you at increased risk of developing a spinal disc herniation.
Cardiovascular factors including high blood pressure are significantly associated with lumbar disc herniation.
Genetic factors can also contribute to slip disc as specific genes may be linked to inherited forms of disc disease
Prolonged hospitalization can also cause increase risk of lumbar disc herniation due to weakness of the supporting muscles from underuse
When should I consider surgery?
If you are suffering from persistent disabling low back pain lasting for more than six weeks, and if you have failed non-surgical interventions like epidural injections, pain medication, and physical therapy, then you may be an ideal candidate for spinal decompression surgery.
If along with the back pain, if you have progressively worsening weakness, numbness and tingling, which is not responding to conservative therapy, then a visit to the surgeon is recommended
If you have developed cauda equina syndrome, which is a rare condition in which the bundle of nerves below the end of the spinal cord get damaged producing low back pain with numbness, a surgical intervention may be warranted. If left untreated, this may lead to loss of control over your bowel or bladder movements
Summary
Spinal disc herniation can be a very painful and debilitating experience but around 90% of patient’s experience improvement in their disc herniation symptoms within three months of conservative care and management with physical therapy being an excellent option. Adopting a healthy lifestyle is essential as well and you should be regular with your fitness and incorporate healthy eating habits so as to keep your weight in check. Consult your physical therapist or pain management specialist for addressing acute exacerbation’s.